You Broke It, You Bought It: Contingency Management and Addiction Recovery

Contingency Management is the practice of paying people to make measurable strides in recovering from substance use disorders. This often takes the form of gift cards in exchange for clear urine samples, attending group therapy, and participating in online check-ups and counseling sessions.
Contingency Management is considered the most effective way to wean people off substance use disorders. Drugs such as naloxone, buprenorphine, and methadone help with withdrawal symptoms but without some form of cognitive behavioral therapy, or CBT, relapse and readdiction are the likely outcomes.
The people with serious substance use disorders are different from daily drinkers or pot smokers or hard-drug curious persons wary of addiction. They have given themselves over to making acquisition of drugs the most important thing in their lives to the point where they are willing to lie, steal, and risk death to continue their habit.
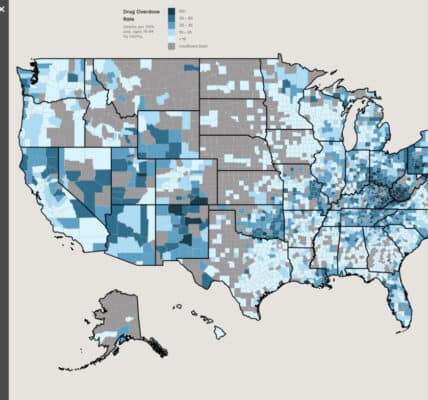
In most cases, serious drug addicts have succeeded in destroying their own lives and damaging many of the people closest to them, those whose help is often needed to recover. They are often unable to hold a job or sustain a committed relationship. They might not be able to afford housing. In the United States in 2024, more than 250 people will die from drug overdoses every day. Many more will take their own lives rather than continue living this way.
What does society say to these suffering souls? Tough luck. There are treatments we know work, and yet fewer than 10% of hardcore drug addicts are in treatment programs. We suspect there are new drugs that will help them, such as GLP-1 agonists like Ozempic and Wegovy. However, the pharmaceutical companies will not run trials because they believe the drugs will be unprofitable. Medicaid won’t pay for the drugs and private insurance companies are beyond the reach of most recovering addicts. As a society, we tell the drug addict: You did this to yourself; either endure white-knuckle withdrawal or die.
How did the opioid addict get there? How did the roughly two million people who suffer from opioid addiction get into this condition? Many were prescribed narcotic medications and have difficulty getting off them. In many cases, their pain persists, so does their desire for opioids. If we cannot stop the pain of injury, isn’t it humane to provide painkillers? Many people can manage their drug use within socially acceptable boundaries if they are taught how to manage pain and medication.
Many people become drug addicts because they were essentially born addicted. Genetics accounts for roughly 50% of opioid addiction, with the genes of newborns impacted by the addictions of their parents and their parents’ parents, etc. Tough luck, society says, providing little care for crack babies who grow up predisposed to substance abuse. What can they do on their own? Plenty, it turns out, as most have shown extraordinary resilience and have helped chart pathways out of addiction.
The hardcore opioid addicts don’t get hooked because of the drugs, writes one of the nation’s leading researchers into addiction and recovery. They get there because of stressful events in their lives that make intoxication attractive. Many suffered abuse, neglect, and injury as children or adolescents. They indulge to escape and forget. Substance abuse calms their anxieties until they realize they have lost control and shaped their lives around it. They need help, not indifference.
If most of the opioid addicts in America are broken people — and a disproportionate number are veterans with psychological issues inflicted by military training and service — aren’t we as a society somewhat culpable and isn’t it our job to fix this? When people oppose Contingency Management because it is paying junkies to stay clean, aren’t we injuring the public good out of spite?
When you look at the effectiveness of paying people to stay in treatment, show up for therapy, take your medications, run clean blood tests and urine tests, isn’t it the best money spent of the billions and billions spent on addiction treatment programs? Yes it is! When you see someone who has been an addict for 35 years, and they run clean urine tests, week after week, for months, isn’t that a miracle of sorts that we should celebrate and replicate?
When you look at the chaotic lives of hardcore drug addicts, you see why other therapies fail. If you first treat the addict for overdose in the emergency room, they are gone as soon as they recover. Back on the street, they are looking for drugs, not therapy. They won’t attend the therapy voluntarily unless they are paid. And then, remarkably, they will attend, for the most pathetic of sums, and a good number will stick it out, pass their tests, and quickly recover to a life where one’s family and future are more important than painkillers.
Don’t we, as a society, owe this compassion to those among us who are so broken they can no longer lift themselves out of addiction? Don’t we all profit when we invest in the recovery and rehabilitation of those who are temporarily a burden to themselves and society? We should be delighted, not resentful, every time an addict swaps a clean test for a gift card. That is a person on their way to a productive future.
Written by Steve O’Keefe. First published July 18, 2024.
Sources:
“S.F. treats meth addiction by paying — and supporting — those in recovery,” San Francisco Chronicle, July 16, 2024.
“A Psychiatrist Breaks Down the Top 5 Myths About Addiction,” Next Big Idea Club, July 15, 2024.
Image Copyright: Rusty Blazenhofff, used under Creative Commons license.