Using Lifestyle Medicine to Treat Illness by Changing Behavior

Lifestyle medicine is a relatively new approach to treating illness with therapeutic interventions for chronic diseases, including heart disease, diabetes, and obesity. The American College of Lifestyle Medicine, which provides certification and continuing medical education, lists the “six pillars of lifestyle medicine”:
- nutrition
- physical activity
- restorative sleep
- stress management
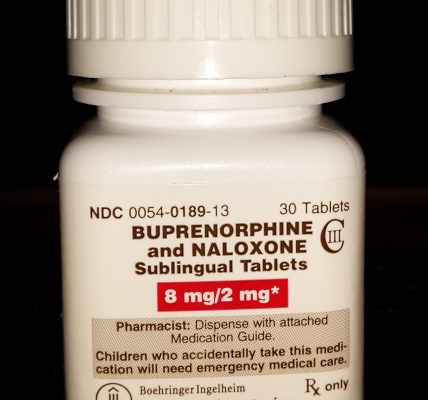
- avoidance of risky substances
- social connection
In 2019, 40 leaders in the field of Lifestyle Medicine (LM) gathered in Philadelphia, Pennsylvania, to help establish research priorities for the new field. At the Lifestyle Medicine Research Summit, they looked at such things as standards of evidence, research methodologies, data analytics, and data modeling with a goal of developing “evidence-based guidelines on lifestyle medicine.”
The biological foundations of lifestyle medicine are explained in vivid detail in this passage from the final report from the research summit:
The health effects of diet, sedentary lifestyle, chronic stress, medications (often used to treat lifestyle-determined conditions), and other aspects of lifestyle (sleep, substance use, emotions and attitudes, positive psychology and social connection) are mediated through common subcellular, epigenetic, and other mechanisms and to create dysbiosis (a state in which gastrointestinal flora become unbalanced or perturbed), cellular stress and injury (often in the form of oxidative stress).
These biological pathways often culminate in the inflammatory response, which then feeds back to drive further cellular stress, dysbiosis, and related epigenetic changes to create a self-sustaining state of chronic inflammation. In turn, chronic systemic inflammation is an early precursor for heart disease; Type 1 and 2 diabetes and depression; and a variety of other endocrine, autoimmune, rheumatologic, and neurological disorders.
There you have LM in a nutshell: If you assess and strengthen these six pillars, you can treat even chronic illnesses successfully. Numerous studies have shown that obesity can be treated with drugs and surgery, but compulsive eating cannot be successfully treated without lifestyle change. The same can be said for many addictions, which can be broken using pharmaceutical interventions, but cannot be cured without lifestyle interventions.
There are many difficulties in assessing the impacts of lifestyle medicine. Researchers point out that it is nearly impossible to organize randomized trials dealing with dietary modifications and other long-term behavior. It is also difficult to narrow down the causes and treatments to one or two pillars. All six must be addressed in tandem, making measurements of their individual impacts difficult.
Researchers have been able to get around these limitations to some degree by tapping into large health datasets and analyzing them through an LM framework. The summit researchers mentioned, in particular, the Framingham Heart Study, the Nurses’ Health Study, the UK BioBank, the Seventh Day Adventist Health Study, the Department of Defense Millennium Cohort Study, the Pittsburgh Study, and the NIH “All of Us” Cohort study as sources for data on the impacts of family, community and environment on chronic illness.
A great place to collect data about the efficacy of lifestyle medicine is the medical community itself. A study of health sciences students in Bahrain found that nearly half of the men and three-quarters of the women reported having no regular physical activity.
While people who study nutrition tend to have better diets, people who study medicine broadly do not have healthier-than-average diets. The Harvard Extension School has offered a class in lifestyle medicine since 2014, both in-person and online. The hope is that medical professionals who take the course will practice healthier lifestyles while also helping their patients to do likewise.
The evidence is in: Changing behavior saves lives, leads to improved outcomes, and is often less expensive and more effective than pharmaceutical interventions at treating chronic disease. This has led to a rapid increase in startup funding for telehealth companies that can deliver effective, remote addiction treatment programs increasingly centered around lifestyle medicine. And there are new studies every day into using behavioral interventions to treat obesity and other diseases. We will be happy to report on them at AddictionNews.
Written by Steve O’Keefe. First published June 6, 2024.
Sources:
“Lifestyle medicine: How doctors are prescribing behavioral changes to reverse illness,” StudyFinds Health & Medical News, June 4, 2024.
“A Web-Based Lifestyle Medicine Curriculum: Facilitating Education About Lifestyle Medicine, Behavioral Change, and Health Care Outcomes,” JMIR Medical Education, November 2017.
“Prioritized Research for the Prevention, Treatment, and Reversal of Chronic Disease: Recommendations From the Lifestyle Medicine Research Summit,” Frontiers in Medicine, December 2020.
Image Copyright: sabbir330.